Is Laparoscopy Necessary for Infertility?
Infertility can be a challenging journey, often filled with questions and uncertainties. Among these is the question: Is laparoscopy necessary for infertility? For many couples trying to conceive, understanding the role of this minimally invasive procedure can be the key to unlocking their path to parenthood.
Let’s break it down and explore when and why laparoscopy might be needed, its benefits, and how it integrates with other infertility treatments.
What Is Laparoscopy in Infertility?
Laparoscopy is a minimally invasive surgical procedure that has revolutionized the way doctors diagnose and treat infertility. By providing a clear and detailed view of the reproductive organs, it allows healthcare providers to identify and address conditions that might be hindering conception.
The procedure involves making a small incision near the navel, through which a thin, lighted tube equipped with a camera, known as a laparoscope, is inserted. This tool not only magnifies the pelvic region for better visibility but also allows doctors to perform targeted surgical interventions when necessary.
Why Is Laparoscopy Used in Infertility?
Infertility often arises from complex conditions that cannot be detected through routine tests like ultrasounds or blood work. Laparoscopy offers a deeper, more precise exploration of the pelvic region, making it an invaluable tool in the field of reproductive medicine.
Here are some of the most common issues that laparoscopy helps identify and treat:
- Endometriosis
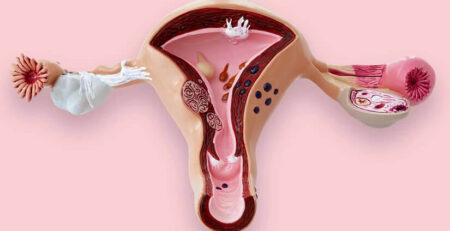
Endometriosis occurs when the tissue that lines the uterus grows outside it, often causing inflammation, pain, and scar tissue. This condition can interfere with ovulation, implantation, or the function of the fallopian tubes, leading to infertility. Laparoscopy not only confirms the presence of endometriosis but also allows the surgeon to remove or destroy the abnormal tissue, improving the chances of conception. - Pelvic Adhesions (Scar Tissue)
Adhesions are bands of scar tissue that can form after infections, surgeries, or conditions like endometriosis. These adhesions may bind the reproductive organs together, disrupting their normal function. Through laparoscopy, doctors can carefully remove these adhesions, restoring the mobility and function of the uterus, ovaries, and fallopian tubes. - Fibroids
Uterine fibroids are non-cancerous growths that can affect fertility by distorting the uterine cavity or blocking the fallopian tubes. Laparoscopy provides a clear view of their size and location and allows for their surgical removal if necessary, especially when they are located on the outer wall of the uterus. - Ovarian Cysts
Cysts on the ovaries, such as endometriomas or dermoid cysts, can sometimes interfere with ovulation or cause hormonal imbalances. During laparoscopy, these cysts can be carefully removed, preserving as much healthy ovarian tissue as possible to maintain fertility. - Blocked Fallopian Tubes
One of the most common causes of infertility is a blockage in the fallopian tubes, preventing the sperm and egg from meeting. Laparoscopy allows doctors to visualize the extent and location of the blockage and, in some cases, clear the obstruction or recommend alternative treatments like IVF. - Combined with Hysteroscopy: This helps to evaluate the uterine cavity and lining of the womb for pregnancy to happen and grow.
Getting pregnant is now easier
Book IVF Consultation
Laparoscopy: A Dual-Purpose Procedure
What sets laparoscopy apart is its ability to serve both as a diagnostic and therapeutic tool. For instance:
- If endometriosis is suspected, laparoscopy can confirm the diagnosis and simultaneously remove the lesions.
- If a blocked fallopian tube is detected, doctors may attempt to open it during the same procedure.
- Similarly if any abnormality is found in hysteroscopy, like polyps, adhesions, septal, fibroids, it is corrected in the same sitting to make lining receptive for embryo.
This dual functionality reduces the need for multiple interventions, saving time and offering patients a more streamlined treatment journey.
How Laparoscopy Improves Infertility Treatment Outcomes?
By addressing physical barriers to conception, laparoscopy can significantly enhance the success rates of natural conception or assisted reproductive technologies (ART) like In Vitro Fertilization (IVF). For example:
- Removing endometrial tissue or adhesions can restore normal pelvic anatomy, improving fertility naturally.
- Treating fibroids or clearing blocked tubes can create a more favorable environment for an embryo to implant, increasing the likelihood of IVF success.
Laparoscopy in infertility is not just a procedure; it’s a window into the hidden causes of reproductive challenges. By uncovering and resolving these issues, it provides couples with renewed hope and a clearer path to achieving their dreams of parenthood.
When Is Laparoscopy Necessary in Infertility?
While not every infertility case requires laparoscopy, it becomes essential in certain situations, such as:
- Unexplained Infertility
When standard tests like ultrasound and blood work fail to identify the cause, laparoscopy can uncover hidden problems, such as mild endometriosis or pelvic adhesions, which are not easily detected through non-invasive methods. - Suspected Endometriosis
Women experiencing painful periods, pelvic pain, or pain during intercourse may have endometriosis. Laparoscopy not only confirms the diagnosis but also allows doctors to treat it during the same procedure. - Tubal Factor Infertility
Blocked fallopian tubes are a common reason for infertility. Laparoscopy can assess the severity of the blockage and sometimes repair the tubes to improve the chances of natural conception. - Repeated IVF Failures
If multiple cycles of IVF (In Vitro Fertilization) have been unsuccessful, Hysteroscopy can check for underlying conditions that might be reducing the effectiveness of the treatment.
How Does Laparoscopy Complement Infertility Treatments?
Laparoscopy plays a pivotal role in enhancing the effectiveness of infertility treatments. While treatments like IVF, ovulation induction, and IUI (Intrauterine Insemination) are designed to address specific fertility challenges, they rely on an optimal reproductive environment to deliver the best results. Laparoscopy and hysteroscopy serves as a bridge, identifying and resolving underlying issues that might otherwise reduce the success of these treatments.
Here’s how laparoscopy integrates seamlessly with infertility treatments:
1- Optimizing the Uterine and Pelvic Environment Before IVF
IVF (In Vitro Fertilization) requires a healthy and receptive uterine environment for the embryo to implant successfully. Laparoscopy and hysteroscopy can identify and treat conditions that might compromise this environment, such as:
- Endometrial Lesions: Removing endometrial tissue ensures the uterus is better prepared for implantation.
- Pelvic Adhesions or Scar Tissue: Clearing adhesions restores the normal anatomy of the reproductive organs, facilitating embryo transfer.
- Blocked Tubes with Fluid Accumulation: A hydrosalpinx (fluid-filled fallopian tube) can leak toxic fluid into the uterus, reducing IVF success rates. Laparoscopy can remove or clip the affected tube to prevent interference.
By addressing these issues before IVF, laparoscopy and hysteroscopy significantly improves the chances of implantation and a successful pregnancy.
2- Enhancing Treatment Outcomes in Severe Cases
Certain infertility conditions require more than hormonal treatments or assisted reproductive techniques. Laparoscopy becomes essential when dealing with severe or complex cases, such as:
- Advanced Endometriosis: Severe endometriosis can cause inflammation, scar tissue, and anatomical distortions that hinder both natural conception and ART success. Through laparoscopy, these lesions are meticulously removed, improving the ovarian and uterine environment.
- Large Fibroids: Fibroids located on the outer uterine wall or within the cavity can disrupt implantation or affect pregnancy outcomes. Laparoscopy allows for precise removal of these fibroids while preserving uterine integrity.
In such cases, laparoscopy doesn’t just complement infertility treatments—it becomes a critical first step that sets the stage for success.
3- Serving as a Diagnostic Tool When Other Tests Fall Short
Infertility can sometimes be a puzzle with no clear answers from initial tests like ultrasounds, bloodwork, or hysterosalpingography (HSG). Laparoscopy acts as a diagnostic game-changer, offering detailed insights into conditions that other methods may overlook, including:
- Mild Endometriosis: Subtle forms of endometriosis that do not show up on imaging can be identified and treated during laparoscopy.
- Adhesions or Minor Tubal Damage: Laparoscopy allows doctors to assess the extent of damage and determine the best course of action.
- Unexplained Infertility: In cases where no obvious cause of infertility is found, laparoscopy often uncovers hidden factors like scar tissue or undiagnosed pelvic infections.
This detailed diagnostic capability ensures that treatments like IVF or IUI are tailored to the patient’s specific needs, maximizing their chances of success.
4- Combining Laparoscopy with Ovulation Induction or IUI
For women undergoing ovulation induction or IUI, laparoscopy can play a supporting role by ensuring that the reproductive system is free of barriers that might impede conception. For example:
- Checking Tubal Patency: Laparoscopy ensures the fallopian tubes are open and functional, a key factor for natural conception and IUI.
- Removing Obstacles: Any physical blockages, cysts, or abnormalities detected during laparoscopy can be addressed, enhancing the effectiveness of these treatments.
5- Increasing IVF Success Rates
For patients undergoing IVF, laparoscopy and hysteroscopy offers several advantages:
- Improved Egg Retrieval: By addressing ovarian cysts or adhesions, laparoscopy ensures better access to the ovaries during egg retrieval.
- Enhanced Embryo Implantation: Clearing fibroids or repairing uterine abnormalities ensures a more receptive uterine lining for embryo transfer.
- Addressing Recurrent IVF Failures: If a patient has experienced multiple IVF failures, laparoscopy can reveal hidden conditions that might have contributed to the unsuccessful outcomes.
Why Laparoscopy Is Often Recommended?
The complementary role of laparoscopy in infertility treatments lies in its ability to provide clarity, precision, and solutions. By resolving issues at the root level, it creates a more favorable environment for any fertility treatment to succeed. This makes it an invaluable tool for couples seeking answers and results on their path to parenthood.
When combined with treatments like IVF, ovulation induction, or IUI, laparoscopy ensures that no underlying condition is left unaddressed, ultimately increasing the likelihood of achieving a healthy pregnancy.
Is Laparoscopy & Hysteroscopy Always the First Step?
Not necessarily. For most patients, non-invasive options like hormonal therapy, timed intercourse, or simpler diagnostic tests are explored first. However, when symptoms or test results suggest a deeper issue, doctors may recommend laparoscopy.
For example, if a woman has chronic pelvic pain or irregular periods, it may point to a condition like endometriosis or adhesions. In such cases, bypassing laparoscopy could delay effective treatment.
What Are the Benefits of Laparoscopy & Hysteroscopy in Infertility?
The advantages of laparoscopy go beyond just diagnosis. Here’s why it’s considered a game-changer in the field of infertility treatment:
- Minimally Invasive: Unlike traditional open surgeries, laparoscopy involves tiny incisions, resulting in faster recovery and minimal scarring.
- Dual Purpose: It allows doctors to diagnose and treat issues in a single procedure, reducing the need for multiple interventions.
- Accuracy: Laparoscopy offers a detailed view of the reproductive organs, providing insights that non-invasive tests often miss.
- Improved Fertility: By addressing conditions like blocked tubes or endometriosis, it can significantly enhance the chances of natural conception or IVF success.
Risks and Recovery
As with any surgical procedure, laparoscopy carries some risks, such as infection, bleeding, or reaction to anaesthesia. However, these risks are minimal, especially when performed by experienced specialists.
Recovery is usually quick, with most patients resuming normal activities within a week. Some mild abdominal discomfort or bloating may occur, but these symptoms typically subside within a few days.
Alternatives to Laparoscopy
If laparoscopy seems daunting, it’s important to discuss alternatives with your doctor. Diagnostic options like hysterosalpingography (HSG) or saline sonohysterography can evaluate certain aspects of infertility. However, these tests cannot address issues like endometriosis or pelvic adhesions, where laparoscopy remains the gold standard.
Final Thoughts: Is Laparoscopy Necessary for Infertility?
The necessity of laparoscopy depends on individual circumstances. While not every infertility case requires it, laparoscopy plays a pivotal role in diagnosing and treating conditions that are otherwise difficult to detect.
For couples facing unexplained infertility, repeated IVF failures, or symptoms of pelvic conditions, laparoscopy can provide clarity and pave the way for successful infertility treatments.
Make the Best of Science and Start Your Journey
If you are struggling with infertility and wondering whether laparoscopy could be the right step for you, consult Dr. Rhythm Gupta, a renowned IVF specialist in Delhi. With her expertise in advanced fertility treatments, including laparoscopy, she can help you find the answers and solutions you need to start your journey toward parenthood. Book your appointment today to take the first step toward your dream of a complete family.

Dr. Rhythm Gupta
Consultant Obstetrician,
Gynaecologist & Infertility Specialist,
MBBS, M.S Obstetrics & Gynaecology
At Excel IVF, we don’t just treat tests and parameters. We partner with you through the emotional, scientific, and medical journey of fertility. Here, Dr. Rhythm Gupta, the leading IVF specialist in Delhi, shares insights from her years in reproductive medicine, breaking down myths, best practices, and what matters most in your path to becoming a parent.
Book a consultation today to understand better and begin your parenthood journey. Call: +91-8920963596 or Email Us: excelivf@gmail.com