Introduction to PCOS: Understanding the Basics
Have you ever heard of PCOS? No?
It stands for Polycystic Ovarian Syndrome. It’s this hormonal thing that many women deal with during their baby-making years. Think of it like this: sometimes our bodies get a little extra male hormones (yeah, women have them too, just in teeny amounts). This can mess up the monthly cycles.
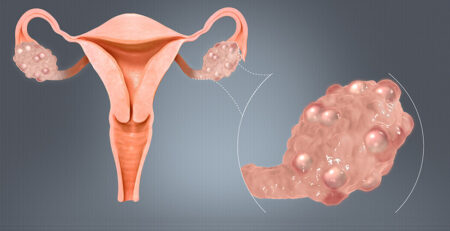
Now, the “polycystic” part? It sounds super sci-fi, but it’s just about our ovaries sometimes having these little water balloon-like sacs called cysts. They’re full of baby eggs that, well, sometimes don’t grow up as they should. It’s like they’re waiting for their moment to come but keep missing the prompt and remain undeveloped. That’s PCOS.
And here’s a little twist: even though it’s in the name, not every woman with PCOS has these cysts.
PCOS affects 8% to 13% of females of reproductive age worldwide. But do you know, according to the World Health Organization (WHO), up to 70% of PCOS cases can go undiagnosed due to the variability of its symptoms and the lack of awareness among the patients? That is definitely the cause of concern and this is where self awareness and medical knowledge come in handy. You would agree!
Now, let us be more aware and get familiar with this prevalent condition in females.
PCOS can cause various health problems, including infertility, weight gain, type 2 diabetes, heart disease, depression and anxiety. Therefore, understanding PCOS for early diagnosis and PCOS treatment is essential. In this blog, we will understand the basics of PCOS, including treatment options.
Signs and Symptoms of PCOS
The interesting thing is that signs and symptoms of PCOS may vary from one woman to another. Sometimes, this also leads to PCOS going undetected. Some women may not experience any symptoms until early adulthood, but others may face symptoms in adolescence. Now, isn’t that a bit of a worry? But it can be tackled, however.
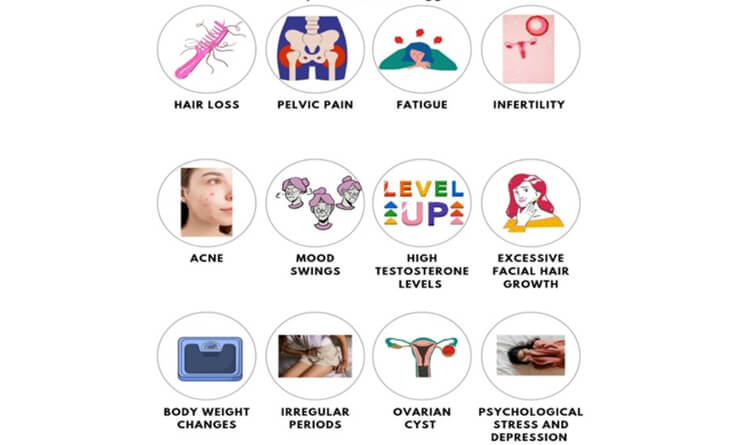
The most common signs and symptoms of PCOS may include:
Irregular Menstrual Cycles: Usually, when you are not pregnant, your body goes through a monthly menstrual cycle. Normally, a regular menstrual cycle typically falls within the 22 to 35-day range. But in PCOS (Polycystic Ovary Syndrome), this whole process gets a bit messy. Instead of having your period like clockwork every month, it becomes unpredictable. Sometimes, you might get it early, sometimes late, and sometimes you might even skip it for several months in a row. PCOS can cause nine menstrual cycles in a year that may last more than 35 days. But why does it happen?
This happens because, in PCOS, your ovaries don’t produce egg. They might make too many tiny cysts (small sacs filled with fluid), and this can change your hormone levels. As a result, your periods become irregular, and it can make it challenging to predict when your next one will show up.
Excessive Hair Growth (Hirsutism): This is another prevalent symptom, a bit disappointing too, yes! In POCS, you might notice extra hair in places where you don’t usually expect it, like your face, chin, or maybe even your chest or back. In PCOS (Polycystic Ovary Syndrome), you might have higher levels of androgens, which are often called “male hormones” because they are more common in guys. These hormones stimulate excessive hair growth. These hairs are thicker and harder than normal.
Acne and Oily Skin: As mentioned earlier, in PCOS, androgens can get a bit overactive like little mischievous kids, which sends the signal to sebaceous (oil) glands in the skin to produce more oil (sebum). This excessive oil gets mixed with dead skin cells and clogs the pores. When the pores get clogged, it’s like a perfect hiding place for acne. So, you might notice more pimples, especially on your face, but they can pop up on your chest, back, or other places too. Acne is common in adolescence, but young women with PCOS tend to experience severe acne.
Weight Gain and Difficulty Losing Weight: Normally, when you eat just the right amount of food and stay active, your body stays balanced. You neither gain nor lose weight dramatically. But for some people with PCOS, it’s like their body is tempted to gain weight more easily.
One reason for this is that PCOS messes with your hormones, called insulin, which helps regulate how your body uses the energy from food. But when insulin isn’t functioning as it should, your body may store extra calories as fat, especially around your belly. And when you try to lose that weight through diet and exercise, it’s like your body resists a bit.
Nearly half of the women gain weight, and if you are already overweight, it can make PCOS symptoms even more severe. So dear lady, keep the weight under check always! It is for the long-lasting good.
Hair Thinning or Hair Loss: In PCOS, while you could grow hair in places you don’t want it, you might also lose hair where you would like to keep it. Here is why it happens.
In POCS, your body releases too much androgen. And guess what? Too much androgen can make your hair follicles sensitive and make your hair fall out easier. Some women may only experience mild hair thinning, while others may experience significant hair loss.
Mood Swings and Emotional Changes: PCOS is not just about physical stuff like irregular periods and unwanted hair growth or hair loss. It can mess with your moods and emotions, too. Yes, that is true! You may feel super happy one moment and then suddenly feel really down or irritable without much warning. Now, why this happens?
The exact cause of mood swings and emotional changes in PCOS is not fully understood; however, several factors, including hormonal changes, insulin resistance, weight gain, stress and anxiety, lead to mood swings in PCOS.
Fertility Issues: You know how some people can have babies easily when they want to, while others might have a harder time? PCOS could be the significant reason behind this.
Here is why. In PCOS, your ovaries can’t release eggs regularly as they should. This can make it tough to get pregnant because, without a released egg, there’s nothing for sperm to meet and make a baby.
But don’t worry, it doesn’t mean you can’t have kids if you have PCOS. Many women with PCOS do become moms, but it might take a bit more time and sometimes a little help from fertility treatments or medications.
Metabolic Disturbances: Your body requires the right balance of food and hormones to work smoothly. But PCOS can mess with how your body handles things. First, your body might have trouble using insulin effectively. High blood sugar can lead to issues like type 2 diabetes and can also affect your weight because it can make you more likely to store fat.
Another thing is that PCOS can mess with your cholesterol levels, making the “bad” cholesterol go up and the “good” cholesterol go down. This can increase the risk of heart problems.
Causes and Risk Factors of PCOS
Causes
Now, we have an understanding of what PCOS is and what are its signs and symptoms. But do you know what causes it?
We are not 100% sure why PCOS happens, but there are a bunch of things that might play a role in it. Here are the causes and risk factors associated with PCOS:
Hormonal Imbalance: Normally, your body has a set of hormones that help everything run smoothly. But in PCOS, these hormones can lose balance. The main culprits are elevated androgen levels (male hormones) such as testosterone and luteinizing hormone (LH). This hormonal imbalance interferes with ovulation, meaning eggs do not mature consistently and are not released from the follicles. This results in irregular periods, meaning they don’t come when you expect them to. Additionally, excess androgens can lead to excessive body hair and acne.
Insulin Resistance: Your body has a natural hormone called insulin that helps our cells use sugar for energy. But sometimes, especially in conditions like PCOS, your cells can become a bit stubborn and don’t respond properly, which increases sugar levels. Now to reduce these increased blood sugar levels, the body needs to produce more insulin.
But here’s the twist. This excessive insulin production increases the production of androgen (male hormones). This hormone imbalance can make it harder for the ovaries to release eggs regularly, leading to irregular periods. It can also cause weight gain and those annoying dark patches on the skin.
Genetic Factors: PCOS can run in families. So, if someone in your family, like your mom or your sister, has PCOS, you might have a higher chance of getting it, too. But it doesn’t mean you’re guaranteed to get PCOS if someone in your family has it; your risk might be a bit higher. Genetics can play a role in how your body responds to hormones and insulin, which are big players in PCOS.
Lifestyle Factors (Diet, Exercise, Stress): Some lifestyle factors like diet, exercise and stress can also contribute to PCOS.
- Diet: What you eat can have a big impact on PCOS. If you eat lots of junk food and sugary drinks, it can mess with your body’s ability to use energy from food properly. This can make you more likely to develop PCOS.
- Exercise: Exercise is like a superhero for your body. If you don’t move much, it’s easier for your body to gain weight and have trouble using energy. This can also lead to PCOS.
- Stress: Stress is like an alarm bell for your body. When you’re super stressed, your body releases hormones that can make PCOS symptoms worse.
Low-Grade Inflammation: Inside your body, you have special soldiers called white blood cells. They are like your body’s defence team. When there’s trouble, like an infection or an injury, they jump into action.
But sometimes, in PCOS, these white blood cells can get a bit too active even when there’s no need. It’s like they’re always on high alert. This is what we call “low-grade inflammation.”
Now, this disturbance inside your body can make your ovaries produce androgens associated with guys. Having too many of these hormones can cause problems, like disturbing your menstrual cycle and even increasing the risk of heart and blood vessel issues. Just be mentally prepared.
How Can You Check if You Have PCOS?
Now, after reading all this mind-boggling information, you must be wondering if you might have PCOS. But just relax. We can dive into that, too, because checking for PCOS is like solving a puzzle because, in some women, you can’t notice any visible signs.
So what is the route then? It is always best to consult with a gynaecologist for a proper diagnosis and to steer clear of all the unwanted problems you do not want, right?
Actually, there is no single test to check if you have PCOS. Your doctor will most likely perform a physical examination, obtain a medical history, and prescribe certain tests to help with the diagnosis.
How is PCOS diagnosed?
If you have two of the following three main signs then it is likely you have PCOS:
- Infrequent, absent, or prolonged menstruation.
- Signs of increased androgen levels, like acne, male-pattern hair loss, or excess hair growth on the face, chin, or body.
- Multiple small cysts on the ovaries on ultrasound
Common Tests and Examinations
After evaluating the visible signs, your doctor may recommend some tests to make sure you have PCOS. These tests may include
Physical Exam: When you go to the doctor, they might want to do a physical exam to check if you have PCOS. The doctor will check the signs of elevated androgen levels by checking the excess body and facial hair, hair thinning on the scalp, acne, and other related symptoms. Your doctor may also check the BMI, which is the weight and height ratio, blood pressure and waist size.
Blood Tests: Your doctor will also recommend some blood tests to figure out if your hormones are in balance or if there are any issues that might be related to PCOS. Common tests include:
- Androgen: Your doctor will perform a blood test to check the hormone level, including androgen (Testosterone, Sex Hormone Binding Globulin, !7 OHP, DHEAS) which tends to be elevated in women with PCOS.
- To diagnose insulin resistance: Fasting Insulin, Fasting blood sugar, 75gm glucose challenge test
- Lipid Profile
- Exclusion of Other Conditions: Your doctor will also perform other tests to rule out conditions that may mimic PCOS like thyroid function to rule out hypothyroidism and prolactin.
Pelvic Ultrasound: Your doctor may also perform an ultrasound to see if there are any cysts on your ovaries. They also check how thick the lining of your uterus is. If your periods are not happening regularly, the lining might look thicker than it should.
Importance of Seeking Medical Advice:
PCOS is like a tricky puzzle that affects your hormones and can cause a bunch of issues like irregular periods, acne, weight gain, and even trouble getting pregnant. So, that’s why it is important to seek medical advice.
Accurate Diagnosis: PCOS can be a bit tricky to diagnose on your own. You might have some of the symptoms but not all of them. Seeing a doctor means they can do some tests, like blood tests and ultrasounds, to confirm if it’s PCOS or something else.
To Get Appropriate Treatment: PCOS treatment is all about getting the right advice and finding what works best for you to feel better. Your doctor will look at the signs and symptoms you have and then design a treatment plan for you. This plan can involve changing your lifestyle, taking certain medicines, or trying out other methods to handle the symptoms and boost your health.
To Prevent Complications: Having PCOS isn’t just about the symptoms you feel. It can also increase your risk of developing other health problems, such as type 2 diabetes, heart difficulties, and uterine cancer.
But here’s the good news: if you find out you have PCOS early and get treatment, it can actually lower your chances of having these extra health problems.
To Get Support: Your doctor can give you advice and be there to help you out. Also, if you need more help, like talking to others who are going through the same issue or talking to someone who’s an expert in helping with feelings and emotions, your doctor can guide you in the right direction.

Impact of PCOS on Health
PCOS can mess with your body in a few ways. PCOS isn’t just about how you feel; it can bring extra health challenges. So, beware of everything if you want to live a healthy life despite having PCOS.
1- Fertility and Pregnancy Challenges
When it comes to having babies, PCOS might cause some difficulties.
- Irregular ovulation: With PCOS, your ovaries do not release an egg every month. This can make it difficult to get pregnant because you’re not having enough eggs for ovulation.
- Miscarriage: PCOS can increase the chance of losing a pregnancy early on. This happens because hormonal imbalances can make it hard for a pregnancy to grow properly.
- Difficulty Conceiving: If you’re trying to have a baby, PCOS can make it a real challenge. The irregular periods and unpredictable ovulation can make it harder to know when’s the best time to try for a baby.
- Preeclampsia: When you’re pregnant with PCOS, there’s a higher risk of a serious problem called preeclampsia. This can increase your blood pressure after the 20th week of pregnancy and even hurt your organs like your kidneys and liver. It’s not good for you or the baby.
2- Increased Risk of type 2 Diabetes
If you have PCOS, you’re more likely to get type 2 diabetes. Here’s why: PCOS messes with something called insulin, which helps your body use sugar for energy. When you have PCOS, your body doesn’t use insulin. So, sugar builds up in your blood, and that can eventually lead to type 2 diabetes.
Your chances of getting type 2 diabetes increase as you get older, if you’re overweight, or if others in your family have diabetes.
3- Heart Health Implications
PCOS doesn’t just affect your hormones; it can significantly impact your heart health. Having PCOS makes it more likely for you to have cardiovascular problems because of hormonal and metabolic imbalances associated with the condition. So, taking care of your heart is just as important as looking after your ovaries when you have PCOS.
- Hypertension: Having PCOS can also raise your risk of high blood pressure. When you have PCOS, hormonal imbalances can disrupt how your blood vessels function, causing your blood pressure to rise.
- Abnormal Cholesterol Levels: If you have PCOS, you’re more likely to have trouble with cholesterol, which can increase the risk of heart problems. Your levels of certain types of fats in your blood, like triglycerides, can go up, and the good kind of cholesterol (HDL) might go down.
- Triglycerides: Triglycerides are like a type of fat in your blood. If they’re too high, they can make it more likely for you to have heart problems. When you have PCOS, these triglyceride levels can be higher than usual, which adds to the chance of heart issues.
4- Endometrial Cancer
Endometrial cancer is a type of cancer that affects the lining of the uterus. Now, if you have PCOS, you have a higher chance of getting this kind of cancer.
The exact reason isn’t completely clear, but here’s what might be going on: PCOS can interfere with your periods, make your body resistant to insulin, cause extra weight gain, and bump up the levels of male hormones in your body. All of these things together seem to increase the risk of endometrial cancer.
Managing PCOS Through Lifestyle Changes
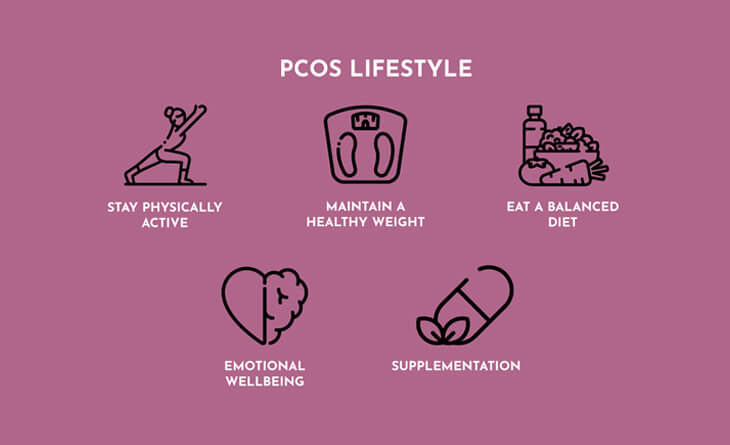
Managing PCOS starts with the way you live. Small changes in your lifestyle can make a big difference. Let’s understand how you can do that.
Importance of a Balanced Diet: What you eat significantly affects your health. A balanced diet is important for everyone, but it is especially important if you have PCOS. You might include whole foods, lean proteins, fruits, and vegetables in your diet and minimise the intake of sugary and processed items. Eating a balanced diet can help you to maintain your insulin level.
Exercise and Its Role in PCOS Management: Exercise is like a superhero when it comes to managing PCOS.
Here’s how it works:
When you’re active, your body gets better at using insulin, which helps control your blood sugar levels. And that’s great news for PCOS patients because insulin issues are part of the problem.
PCOS can make it easier to gain weight. Exercise helps you burn calories, build muscle, and lose fat. This is like hitting the “reset” button on your body, which can help with PCOS symptoms.
PCOS can increase the risk of heart disease. If you exercise regularly, it will reduce your chances of problems like high blood pressure and cholesterol.
Stress Reduction Techniques: Stress can make your PCOS symptoms worsen. When you’re stressed out, you might crave comfort foods that aren’t the best for managing PCOS symptoms. Plus, stress can disturb your sleep cycle, and we all know how important sleep is for managing PCOS.
So, what can you do about it?
- Meditation is like a mental spa. When you meditate, you calm down, worry less, and just feel more emotionally balanced.
- Have you ever noticed how taking a few slow, deep breaths might help you relax? This is because it relaxes you and decreases your heart rate. Simply inhale gently through your nose, hold for a second, then release slowly through your mouth. Repeat many times.
- Gentle movements and stretching can help you relax your muscles and quiet your thoughts. It’s like giving your body a relaxing massage from within.
- Exercise is not just about physical health; it’s a stress-buster, too. Moving your body releases feel-good hormones (happy hormones) that can lift your mood and help you relax.
Medical Treatments for PCOS Depending Upon the Symptoms
When it comes to treating PCOS, changing lifestyle only does not work. Because PCOS is a challenging hormonal disorder with various signs and symptoms. So, it’s better to consult a doctor. Your doctor will evaluate your symptoms and prescribe a treatment plan based on your symptoms.
Anti-Androgen Medications: If androgen is the cause of PCOS, then your doctor may prescribe some anti-androgen medicines like spironolactone, flutamide, and finasteride. These medications block the effect of androgens and help to control acne and unwanted hair growth on the body (hirsutism). These medications may also help you to manage the lipid level, which is elevated in POCS.
But here is something that you should know: If you are pregnant or planning to conceive, then these medications are not good for you.
Hormonal Birth Control: If you have irregular periods in PCOS, then your doctor will prescribe hormonal birth control. This hormonal birth control will help you regulate the menstrual cycle, reducing androgen levels and improving the symptoms of PCOS, like acne and unwanted hair growth.
You’ve got some choices here: there are birth control pills, patches, shots, a ring you put in your vagina, or a tiny device called an IUD that goes in your uterus. They are all ways to stop pregnancy if you’re not planning to have a baby in PCOS, and they also lower the chance of getting a certain type of cancer in the uterus.
Metformin and Insulin-Sensitizing Medications: Metformin is a powerful drug that is commonly used to treat type 2 diabetes, but it also helps with PCOS. Here’s how it works:
PCOS causes insulin resistance in your body. Metformin and other insulin-sensitizing medications improve insulin resistance. And guess what? Improved insulin resistance can help to reduce your elevated androgen levels, regulate your periods, and help you with weight loss.
Fertility Treatments: As we have discussed earlier PCOS can increase the risk of infertility. But that doesn’t mean you can’t get pregnant. If you have PCOS and are trying to conceive a baby, consult your doctor. He/She will recommend an effective treatment plan. The fertility treatment plan includes IVF (in vitro fertilization), IUI (Intrauterine insemination), and ovulation stimulation medications.
Egg-Forming Medicine/ injections: When you’re trying to have a baby, and PCOS is causing trouble with your eggs, doctors can give you special medicines. These meds are like a gentle push for your ovaries to release eggs when it’s baby-making time.
These medications, including Clomiphene Citrate and Letrozole, are taken orally. If this doesnt work, then your doctor will prescribe injections known as gonadotropins. This is often used with other fertility treatments, such as follicle monitoring, intrauterine insemination (IUI) or in vitro fertilization (IVF).
Follicle Monitoring: Follicle monitoring is like keeping an eye on the eggs in your ovaries, and it’s usually done with an ultrasound. When you have PCOS and you’re trying to get pregnant, this monitoring helps your doctor to figure out the best time for those eggs to pop out of the ovaries. It’s like a fertility roadmap to help you know when it’s the right time to try for a baby.
Injections: If treatments like clomiphene or metformin don’t work, your doctor might suggest something else. They can give you shots of hormones called gonadotropins, like FSH and LH. These hormones can help your body release eggs and boost your chances of getting pregnant. It’s like giving your baby-making system a little extra push when it needs it.
Laparoscopy: Sometimes, when lifestyle changes, birth control pills, or fertility medications don’t work for PCOS, your doctor might suggest a surgery called laparoscopy. During this surgery, your doctor will make small holes in your ovaries to help lower the production of androgen hormones. It can also make your periods more regular and improve how your body handles insulin.
IVF: IVF (in vitro fertilization) is the more advanced fertility treatment for women with PCOS who desire to get pregnant. In IVF treatment, medications are given to stimulate the ovaries to produce multiple eggs. Then, these eggs are removed and fertilised with the sperm outside the body in the laboratory under controlled conditions. The formed embryo is transferred to the uterus. IVF can be successful for women with PCOS. The success rate of IVF for women with PCOS can vary depending on several factors, including the woman’s age, the severity of her PCOS, and the quality of her eggs.
Supplements that Help with PCOS
Supplements are often considered complementary options to help manage PCOS by regulating hormonal levels, insulin resistance and inflammation associated with PCOS. There is no one-size-fits-all answer to this question, as the best supplements for PCOS will vary depending on the individual’s symptoms. However, some of the most commonly recommended supplements for PCOS include
Inositol: Inositol is a type of natureceutical that helps to improve insulin sensitivity and ovulation in women with PCOS. So take it and prepare to be a mother.
Chromium: Chromium is a mineral that helps to stabilize insulin resistance by regulating blood sugar levels. It also helps with PCOS by improving BMI (body mass index). Stay fit. 9
Zinc: Zinc is a trace element that can boost fertility by regulating insulin and testosterone levels. Zinc supplements also help to reduce unwanted hair growth in PCOS. You can add red meat, beans, tree nuts, and seafood to your diet to get more zinc. Bonus: It is good for the skin too!
Omega 3 Fatty Acids: Omega 3 fatty acids have anti-inflammatory properties that help to reduce PCOS inflammation and regulate glucose metabolism. Studies have demonstrated that fish oils containing omega-3 fatty acids help to improve ovulation. Want to be a mommy?
Berberine: Berberine is an herbal extract that helps with PCOS by hormonal levels, inflammation, insulin levels and high cholesterol. Keep your body healthy.
Cod Liver Oil: Cod liver oil is rich in vitamins D and A, along with significant quantities of omega-3 fatty acids. These fatty acids have the potential to enhance menstrual regularity and aid in reducing abdominal fat. Want to wear those great-looking dresses?
N-acetylcysteine (NAC): N-acetylcysteine (NAC) is an antioxidant that may help improve fertility and insulin sensitivity and reduce androgen levels in women with PCOS. Who wants that annoying hair here and there?
Chromium: Chromium is a vital trace mineral that helps with PCOS by regulating blood sugar levels and improving insulin sensitivity. Diabetes is not good, after all.
Magnesium: Magnesium is involved in more than 300 enzyme reactions within the human body, including those related to glucose metabolism. Eat well, stay well!
Folate: Folate is important for reproductive health and may benefit women with PCOS, especially those trying to conceive. Just because being a mommy is so good.
But remember, do not just gobble up. Always talk to your friendly doctor before consuming anything because these supplements can interact with the medications or pose side effects. Your doctor will prescribe the right dosage to manage the PCOS symptoms.
Myths and Misconceptions about PCOS
There are several myths and misconceptions about Polycystic Ovary Syndrome (PCOS) that can lead to misunderstandings and misinformation. Here are some common myths and the truths that debunk them:
Myth 1: All Women with PCOS have Ovarian Cysts – Who said that?
Fact: Many women get confused with its name, Polycystic Ovary Syndrome (PCOS), that it is related to cysts. However, many women with PCOS have tiny follicles in their ovaries, which can appear like a “strand of pearls” during ultrasound examinations. These follicles may resemble small cysts, but they are not cysts. These follicles are non-cancerous and typically do not cause pain.
Presence of a cyst is just one of the potential characteristics of the condition, and it is combined with other symptoms, hormonal imbalances, and other criteria to diagnose PCOS. Meet your doctor for correct information, always!
Myth 2: Women Diagnosed with PCOS Can’t Get Pregnant – Um No!
Fact: While women diagnosed with PCOS can have difficulty conceiving naturally due to irregular ovulation, they can still get pregnant. Several fertility treatment options, like egg-forming medications, injections, IVF treatments, and changing lifestyle, can help conceive.
Myth 3: An Irregular Menstrual Cycle Means You Have PCOS – Really?
Fact: While irregular menstrual cycles can be a symptom of PCOS, but not exclusive to this condition. Normal menstrual cycles typically fall within the range of 21 to 35 days. Many factors can contribute to irregular periods, including stress, weight fluctuations, hormonal imbalances, and other underlying medical conditions. If you are experiencing irregular cycles, it’s advisable to consult your gynaecologist. He/She will perform additional tests and examinations to pinpoint the underlying cause.
Myth 4: Women with PCOS Can’t Lose Weight – Absolutely Wrong!
Fact: Women with PCOS can find it difficult to lose weight, but it is not impossible. Weight management is entirely possible for women with PCOS through a combination of a healthy diet, regular exercise, and, if needed, medical guidance and support. Weight loss can help improve PCOS symptoms and overall well-being.
Myth 5: PCOS Only Affects Overweight Women – Not at all, dear!
Fact: It is true that being overweight is a significant symptom of PCOS. However, PCOS does not selectively target women based on their body size, and it is rather of two types Obese PCOS & Lean PCOS. Insulin resistance can cause PCOS in women, which results in weight gain. Therefore, adopting a routine of healthy eating and regular exercise is typically advised as an integral part of the PCOS treatment plan for most women with PCOS.
Myth 6: All Women with PCOS Experience Unwanted Hair Growth – Not true entirely!
Fact: Excessive hair growth (Hirsutism) on the face, back, chest, abdomen, and thighs can be an underlying sign of PCOS, but not all women with PCOS will have this symptom.
Myth 7: PCOS Can’t be Cured – Only one side of the coin!
Fact: PCOS is manageable, and PCOS treatment options, like birth control pills, anti-androgen medications, and insulin-sensitising medicines, are available to address its symptoms and associated health risks. Lifestyle changes and medications can effectively improve the quality of life for those with PCOS.
Do you know what is the best way to steer clear of the myths and misconceptions? Educating oneself about PCOS and obtaining expert advice. Reach out for correct information and learn suitable PCOS management.
Preventing PCOS and Early Detection
Now that we have spoken and discussed so much about this menace troubling a lot of women, let us now find out how it can be prevented. We just do not want it right?
Prevention:
- Maintain a Healthy Lifestyle: Maintaining a healthy lifestyle is one of the most effective methods to lower the risk of PCOS. This involves eating a well-balanced diet along with exercise. Obesity and insulin resistance are frequent symptoms of PCOS, and lifestyle choices can impact both. A diet rich in fruits, vegetables, whole grains, lean meats, and healthy fats can help control insulin levels and lower the risk of PCOS. Similarly, regular exercise can enhance insulin sensitivity, help lose weight, and promote hormonal balance. So go for that run today! Or YOGA!
- Eat a Healthy Diet: Diet is important in PCOS prevention. A well-balanced diet promotes healthy weight maintenance and helps in blood sugar regulation. Also, a healthy diet can help to improve insulin sensitivity and regulate hormones. Reducing your intake of processed meals, added sugars, and carbs with a high glycemic index can be very beneficial. To avoid blood sugar spikes, focus on whole meals and fibre-rich foods with a low glycemic index. So check your plate at all times! It is important!
- Exercise Regularly: Obesity is linked to PCOS, and reducing extra weight can be useful. Even a small weight loss might contribute to improvements in PCOS symptoms. Losing weight can help regulate menstrual cycles, lower androgen (male hormone) levels, and improve fertility. Aim for at least 30 minutes of moderate-intensity exercise, like running and jogging, to manage weight daily. Are you starting today?
- Manage Stress: High stress levels may worsen PCOS symptoms. Stress-reduction techniques, such as meditation, yoga, deep breathing exercises, and mindfulness practices, can be beneficial in managing stress levels. Finding healthy ways to cope with stress is important to PCOS prevention. Got a hobby that makes you happy? Pick it up 2-3 times every week.
How can you detect PCOS at early stages?
Now this is very important you see. Early detection of PCOS can help to prevent complications such as infertility, diabetes, and heart disease.
- Menstrual Irregularities: One early sign of PCOS is irregular menstrual cycles. Signs like changes in the length of your menstrual cycle, missed periods, heavy bleeding, or unusually long cycles should not be ignored because these irregularities can indicate hormonal imbalances associated with PCOS. 2-3 missed periods? Consult a gynaecologist immediately.
- Symptom Awareness: Familiarise yourself with common PCOS symptoms like acne, hirsutism (excessive hair growth, particularly on the face), unexplained weight gain, and hair loss. While these symptoms can be related to various causes, experiencing them in combination, especially with irregular menstrual cycles, could be a sign of PCOS. Keeping track of these symptoms and discussing them with a doctor can lead to early diagnosis. Seeing unusual hair growth? It is time for a check!
- Regular Check-Up: Regular check-up is essential if you have a family history of PCOS. During routine check-ups, your doctor will assess your overall health, discuss any concerns you may have, and perform necessary tests to monitor your well-being. Book the body profile every six months.
- Hormone Testing: If you suspect PCOS or have risk factors, your doctor may advise you to get a blood test to check your hormone levels. Elevated androgen levels, such as testosterone, and abnormalities in other hormones can be signs of PCOS. Make sure of everything.
- Pelvic Ultrasound: A pelvic ultrasound may help visualise the ovaries and detect cysts or other abnormalities, which helps in PCOS treatment. While not all women with PCOS have visible cysts, this imaging can help with diagnosis and early detection. It is always good to be aware.
- Metabolic Testing: If you have unexplained weight gain or skin abnormalities (such as dark spots on your skin), your doctor might recommend metabolic testing. This can involve glucose tolerance testing and insulin level assessments, which may help identify insulin resistance, a typical indicator of PCOS. Take a good look at yourself today!
- Consult a Specialist: If you suspect PCOS or are experiencing symptoms related to the illness, you should see a gynaecologist, endocrinologist, or reproductive specialist specialising in PCOS. These experts can give a more thorough review and specialised advice. Also, a doctor can always prove to be your best friend.
Final Words!
It is undeniable that PCOS is a complex disorder that occurs due to hormonal imbalances and irregular menstrual cycles and has potential consequences for an individual’s health. It is a condition that affects a significant portion of women of reproductive age. However, understanding the basics of PCOS, including its definition, prevalence, key symptoms, and potential long-term health risks, lays the foundation for informed decision-making and proactive management. Be smart and live smart!
If you or someone you know is experiencing PCOS symptoms or seeking guidance on its management, make sure to meet Dr. Rhythm Gupta, an experienced gynaecologist and infertility expert with expertise in PCOS and IVF treatment. She can provide personalised advice, diagnosis, and PCOS treatment options to help people effectively manage PCOS and improve their quality of life. Be happy, stay smiling!